Last week, I was privileged to speak at the 'Making a difference to children and young people’s mental health and wellbeing' session at the National Children and Adult Services Conference in Bournemouth.
The session, and the preparation leading up to it, provided an opportunity to review what has been achieved in recent months on our journey to develop and improve mental health services for children and young people. Not because services feel drastically better or different for those using them - yet - but because it feels we are now on the path to improving the lives of many people, the beginning of a significant shift that will change the way that services are organised, provided and regarded for the better.

I was struck that it is just over six months since we published Future in mind – the previous Government’s report of the Children and Young People’s Mental Health and Wellbeing Taskforce. The report and what it represents was the result of genuine collaboration, and not just with the leaders of organisations that you would expect, but also charities, young people who’ve directly experienced the mental health care system (the good bits and the not so good), their parents, and professionals, including social workers, teachers and psychiatrists.
The taskforce took on board the views of more than 1,600 children and young people, over 400 parents and hundreds of health professionals, to inform the findings of the report and proposals – all captured in Future in mind – on how to improve young mental health care in this country. I urged attendees in the room to read the report, as I also urge you to read it if you’ve not done so already.
When the report was published on 17 March, there was positive recognition from much of the young mental health sector about what it represented. There was also some fair challenge back to government that - what really mattered - was not the paper it was printed on, but how soon it would become a catalyst for more effective, simplified and impactful mental health services responding to what young people tell us they need.
During this conference session, I spoke to attendees, alongside my NHS England colleague, Clinical Director, Dr Jacqueline Cornish, about the things happening now as a result of the Taskforce’s proposals. Local areas have been busy developing their transformation plans that will not only give us a rich picture of the local ambition to improve services, but will also be a vehicle for bringing transformed young mental health services to every part of the country. This will not be a one-size-fits-all approach, but one that responds to the particular needs of each area.
Earlier in the summer, we announced the distribution of the first slice of money from the £1.25bn that was set out in the spring budget for CYPMH services. That funding has been made available over the course of this Parliament for spending on children and young people’s mental health, of which we are spending £143 million in this tranche. Another £30 million will be spent this year on improving services for those with eating disorders.
We are commissioning a new national prevalence survey that will provide us with up-to-date data and aid more intelligent and informed decisions about local care approaches, matched to the level of need. We are also developing plans for anti-stigma work aimed at young people and access to better digital information and advice that helps people to understand what they’re experiencing and how to help themselves, or find a service that can.
Rhys Hart, Chair of the Youth Select Committee (YSC), was co-chair of our session panel and provided valuable insight from a youth perspective. The YSC will be publishing their own recommendations next month and I look forward to seeing their report when it is published. Also speaking were staff from Chatterboxes – a youth-led project run by the Bournemouth YMCA, which supports disabled young people, promotes creative approaches and provides friendship.
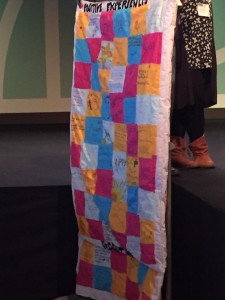
A young woman who had struggled with post-traumatic stress disorder and has Asperger’s, who used the service in Dorset, presented a patchwork quilt, featuring fabric squares depicting individuals’ various experiences. The process of making the quilt was one that encouraged young people to share their voices and she gave her own moving account of the impact the Chatterboxes project has had in her life.
Further speakers – a community engagement lead from the local Dorset Healthwatch and a Director of Commissioning from Derby County Council – provided their insights and ideas: the benefits of recent community investment work to train up young peer mentors, for example; the continuing need to up-skill the workforce so that it’s not just ‘mental health professionals’ who know what to do; and both reiterated the need to listen to young people and prioritise plain, clear language over unnecessary clinical speak and jargon. And crucially, to assume this is just about how to improve mental health services is to miss the point. This is about whole system transformation, making sure prevention and resilience building is part of local service provision.
As we seek to make progress, we must be transparent about what we’re doing and the money being invested. We must strive across the country to improve access and waiting times. We must embed better mental health skills and capacity in primary care, in schools, in children’s centres and in youth centres. And, above all, we must continue to listen to young people to make sure we are approaching our system changes in the right way.
